IBS (Irritable Bowel Syndrome) is a common gut disorder that affects millions of us around the world. It could even affect up to as many as 1 in 3 of us in the UK (according to Guts UK). But even though lots of people experience IBS symptoms, many don’t seek the help and advice they deserve.
Here’s the lowdown on the 4 different types of IBS – and how you can start getting on top of symptoms.
First, a quick recap. What is IBS?
IBS is described as a disorder of the gut-brain connection, where the communication between the gut and brain isn’t working smoothly. This means your gut can be super sensitive (aka hypersensitivity), so certain foods can trigger tummy troubles.
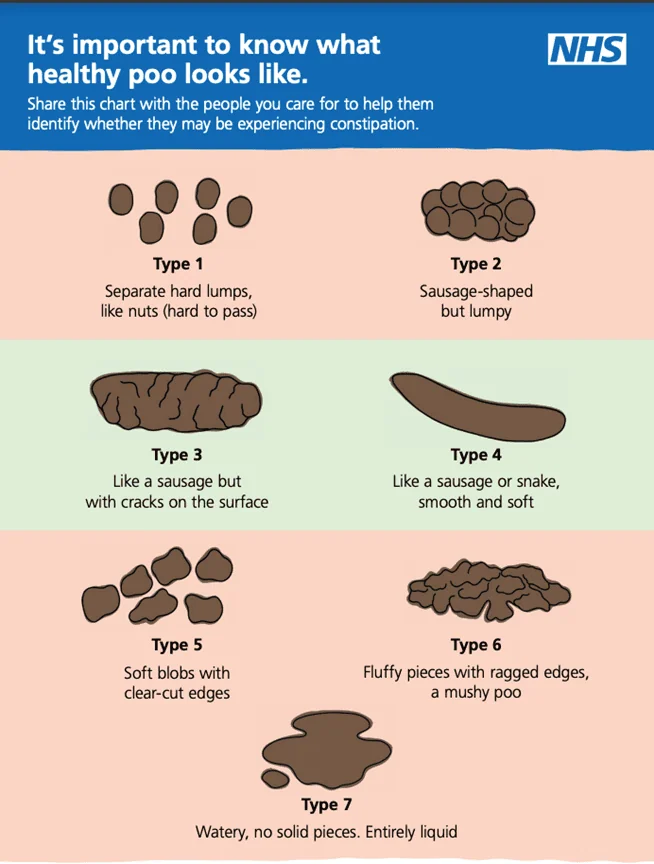
This can look different for different people. But the common complaints are tummy pain, bloating, gas and a change in bowel habits. There can also be feelings of urgency (you need to go *right this second*) or incomplete evacuation (when you don’t feel like you’ve completely emptied). Other symptoms can include heartburn and reflux, as well as headaches, anxiety and fatigue.

 Written by
Jo Cunningham RD
Written by
Jo Cunningham RD